By: Beth Andersen
When we visited my father Lyle Andersen at a life care center in Bozeman, Montana, in late December 2021, we did not know that within a day or so we would receive a call that he had gone into hospice. I did not know it would be the last time I saw him before his life ended on Jan. 2, 2022. He was 86 years old.

Visiting my father, Lyle, in December 2021.
The cause of death was a broken hip bone but also the culmination of a long and valiant struggle with dementia – his mind and then his body slowly breaking down.
How Dementia Affects Individuals
In the case of Alzheimer’s disease, which may or may not have been my father’s condition, the disease begins by destroying memory-related neurons and their connections in the entorhinal cortex and hippocampus. It later affects areas in the cerebral cortex responsible for language, reasoning, and social behavior. Ultimately, it is fatal. (See National Institute on Aging, U.S. Dept. Health and Human Services, “What Happens to the Brain in Alzheimer’s Disease?”)
I witnessed my father’s loss of cognition affect the place of his highest level of thinking. The brilliance with mathematics (he was a tenured math professor), the quick wit, the sage advice, the lifetime of memories and knowledge of what made each member of our family so uniquely known and loved by him.
In his last years, instead of calling me by name or even knowing I was his daughter, my father would say things like “I know you. You are a nice person.”
That was not even the hardest part for me. What was harder for me was realizing that a person can literally live for years as a different person who is no longer in control of their thoughts, can no longer access their memories, is seriously impaired. Who are we when we lose our “mind” so to speak in that manner? Come to think of it, who ARE we really? And, of course, the thoughts that this could happen to us.
Alzheimer’s Disease, Dementia and the Family
Alzheimer’s disease is the seventh leading cause of death in the United States, although some think it may be as high as third or fourth leading cause after heart disease, cancer and COVID. (See Center for Disease Control, Leading Causes of Death, Mortality in the United States 2020.) Other dementias include Lewy body dementia, frontotemporal disorders, and vascular dementia or a combination of two or more types of dementia. (See National Institute on Aging, U.S. Dept. Health and Human Services, “What Happens to the Brain in Alzheimer’s Disease?”)
The Economist characterized the rising prevalence of dementia as a global emergency, stating that almost 2 percent of 65- to 69-year-olds have dementia and the risk of developing it doubles every five years after that. At present, about 50 million people around the world have the condition, a number expected to rise to 82 million by 2030 and 150 million by 2050. Most of the new cases are in the developing world, where populations are rising and aging.
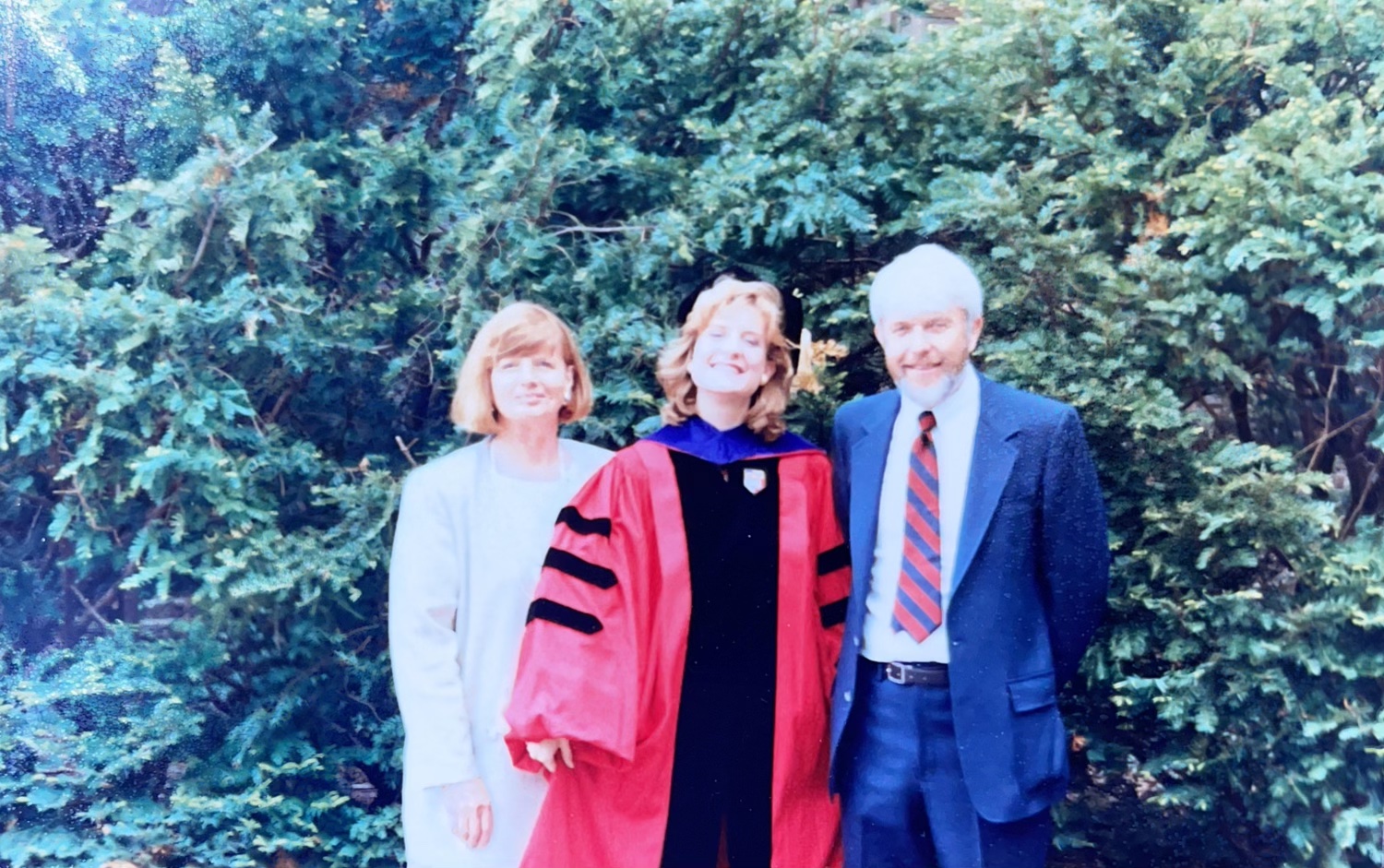
My parents and I celebrating my graduation from Cornell Law School in 1988.
As tough as witnessing my father’s decline may have been, the effect on my entire family, and especially my mother, was one of the most difficult challenges. My mother was his full-time caregiver. As the disease progressed, he kept her on her toes from sunup to sundown as If caring for a newborn. And when the time came for him to live full-time in a care facility, that was hard too. We no longer knew what was happening and we missed him. We could not control much of his day-to-day. It was always a surprise when the next time we saw him, he no longer wore a beard or had abandoned his favorite Montana State University hat for someone’s Arizona hat featuring a cactus.
The fact is that caregiver burnout, financial hardship, physical risk, legal issues, emotional trauma and other hardships can arise when a family member suffers from dementia. Being proactive can help the entire family weather this storm without being devastated.

My dad and his father after my dad graduated with his PhD from Denver University.
How to Prepare for and Address Dementia in a Family Member
For my family, fortunately, my parents had a great estate plan in place. This made the transition so much easier. Here are some pointers I would like to share for those who have a family member who is facing dementia.
- PLAN AHEAD: Medicaid has a five-year look-back. You want to have a Medicaid Trust and any conveyances of property in place at least this far in advance to preserve that eligibility down the road. In addition, the impairments may increase over time such that the person is no longer sufficiently competent to do their own estate plan.
- PREPARE ESTATE PLANNING DOCUMENTS: It is important that the person facing dementia has a will, living will, medical and financial powers of attorney, and in some cases also a trust. Financial Planner Kevne Sharpe also provided me with a dementia planning document. Just make sure to share the dementia planning document with your lawyer so it is consistent with any other planning documents you prepare. For those in Colorado, give me a call at Andersen Law PC at 720-922-3880 or on my cell at 303-808-4794 and I will happily give you a free consult on the estate planning documents best for your family and you.
- GET A DOCTOR’S NOTE BEFORE PREPARING ESTATE PLANNING DOCUMENTS: A person facing dementia may not realize their level of impairment and even family members may be unsure. Also, due to degenerative nature of the condition, things change. A doctor’s note will be evidence that the person preparing the documents is competent to do so. See also our blog on Why You May Want a Doctor’s Note as Part of Your Estate Plan.
- HAVE ONGOING CONVERSATIONS WITH ALL FAMILY MEMBERS AND THE PERSON FACING DEMENTIA: Despite the impairment, the person at issue will want to be involved as much and as long as possible and to be treated with respect. Facing mortality and a loss of autonomy — issues like giving up driving privileges or needing in home or residential care — are difficult. But this person is still alive and may have opinions that are valid and important to them. Even if not, if the progress is such that they cannot weigh in, they should be respected and included to the extent possible.
- HAVE ONGOING CONVERSATIONS WITH ALL FAMILY MEMBERS: So too ALL family members need to have difficult conversations to ensure everyone is on the same page. Our family’s conversations were sometimes awkward and difficult, even involving misunderstandings and a range of emotions. Nonetheless, we persevered and worked things out as a team. For this reason, after our father’s passing, my mother, brothers and sister, in-laws and children are all on the same page, getting along better than ever.Meanwhile, in other families, people do not talk things over because it was so awkward. Totally understandable but not a good idea. Failing to have a conversation can lead to resentment, anger and hurt later. A typical problem is when the person doing a greater share of the ongoing work and caretaking receives or expects a larger voice or inheritance. Address expectations in order to be sure everyone understands and will follow the plan. Do NOT make assumptions. Ultimately, make compromises, perhaps being a bit more fair and bit less greedy than you think justified because, in the end, no family member is 100% objective when it comes to their family and their own contributions.
- LOOK OUT FOR DISINHIBITION AND SWOOPERS: With dementia comes a loss of cognition and impulse control. Suddenly, a calm introverted person may become a compulsive gambler, internet shopper or investor, serial dater getting catfished on a dating site or taken to the cleaners by a so-called friend, acquaintance or even relative. I call people who exploit someone dying or impaired “swoopers” because they swoop in like vultures at the end to take away as much as they can get. Many times, I am called in when someone with dementia has gifted or spent $70,000 or more. Get involved earlier before this happens, asking to “help out” and look at financials and documentation. If you find someone has been exploited, you can reach out to Adult Protective Services, 720-737-4909. (See also Jefferson County Senior Fraud Hotline 303-271-6980.)
- LOOK INTO CARETAKING OPTIONS: It is important to look into in-home and residential caretaking BEFORE it is a necessity. You may want to attend Jefferson County Senior Law Day (if it resumes post-COVID) or reach out to local providers of in-home and residential care. See also AARP, “How to Hire a Caregiver” and Consumer Reports, “How to Hire In Home Care.” You may even want to hire an ombudsman or expert to help you find the right facility for your loved one.
- CARETAKE THE CARETAKER: Do not ignore the needs of the person caring for a person with dementia. Offer to help them organize or take a day for themselves. Nonprofits and support networks can be a big help. See, for example, local chapters of the Alzheimer’s Association.
- ENJOY THE NOW: As my children grew, I made sure that my wistfulness for the babies they once were did not prevent me from enjoying the wonderful children and later young adults they had become. Each new stage had something worth celebrating. With my father, I felt the same. I did not want to spend so much time bemoaning the loss of his sage advice that I overlooked how much fun we had playing ping pong and going out for dinner. Later, I did not want to bemoan his forgetting my name so much that I missed out on the fun of drawing pictures and singing, “You Are My Sunshine” together at the life care center. In my last visits, I saw him as a shadow of himself, but still enjoyed walking him through the halls and getting those last hugs. I am happy that for some reason, I knew to enjoy the “now” while it lasted. I guess I learned it from my parents.